Vasectomy: Your Questions Answered
Having a vasectomy is a step that should be carefully considered because it’s a permanent form of birth control. (It’s true that vasectomies can be reversed, but doing so requires a second, more involved procedure.) The following Q&A goes over many of the questions many men have as they’re contemplating having a vasectomy.
What happens during a vasectomy?
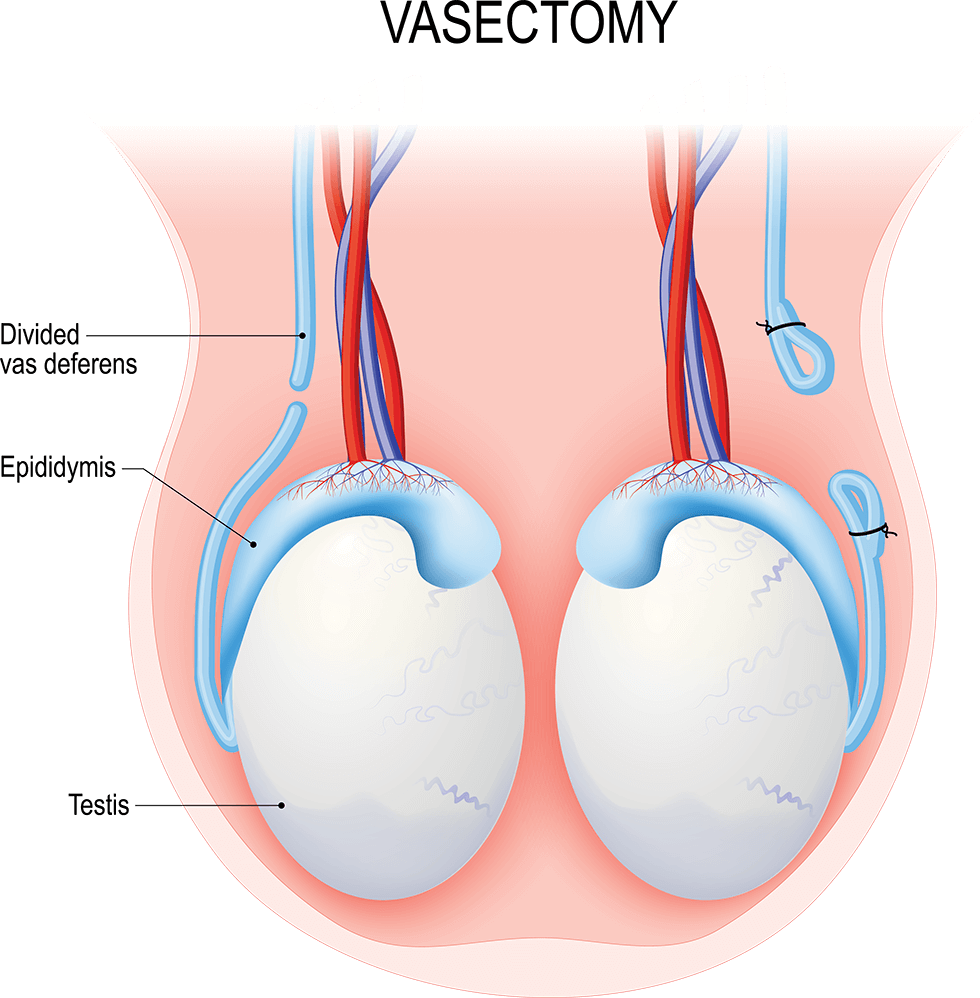
A vasectomy is a simple surgical procedure done to prevent pregnancy. It involves cutting two tiny tubes called the vasa deferentia. (One tube is called a vas deferens or vas.)
Typically, sperm cells travel through the vasa deferentia before they’re mixed with semen and ejaculated out of the body. By cutting these tubes, the sperm cells’ path is blocked. Instead of being ejaculated, the cells are absorbed by the man’s body.
What is a conventional vasectomy?
During a conventional vasectomy, the surgeon accesses the vasa deferentia through one or two small incisions in the scrotum, the sac that holds the testicles. After the vasectomy is done, the scrotal incisions are closed with dissolvable stitches.
What is a no-scalpel vasectomy?
With a no-scalpel vasectomy, the puncture heals on its own, and no stitches are necessary.
With a no-scalpel vasectomy, the surgeon accesses the vasa deferentia through a tiny puncture made in the scrotum. The puncture heals on its own, and no stitches are necessary.
How effective is a vasectomy?
After it takes effect, a vasectomy is about 99.95% effective in preventing pregnancy. This success rate makes it the second most effective form of birth control available. (The first is abstinence—not having sex at all.)
Where are vasectomy procedures done? How long do they take?
Most vasectomy procedures can be done in a urologist’s office. Occasionally, they may be done at a surgical center or hospital. They take about a half hour, and men can go home the same day.
Is a vasectomy covered by health insurance? How much does it cost?
Vasectomies are often covered by health insurance in the United States. A man should check with his insurance company for details on his specific coverage and his out-of-pocket costs. Costs can vary depending on location and the type of surgery needed.
Does it hurt to have a vasectomy?
Men are given local anesthesia (the area is numbed), so there shouldn’t be any pain. There might be some minimal discomfort after the anesthesia wears off. This can usually be managed with ice packs (placed over clothing) or acetaminophen (Tylenol). Aspirin or ibuprofen are not recommended, as they raise the risk of bleeding or bruising.
Can there be complications after a vasectomy?
All surgical procedures have some risk, but complications after a vasectomy are rare. In fact, the American Urological Association notes that complication rates are around 1% to 2%. Complications can include the following:
- Sperm granuloma. When a vas deferens is cut, stray sperm cells can leak out. The immune system responds, which can lead to inflammation and, eventually, a small mass called a sperm granuloma. The mass is benign (not cancerous). A sperm granuloma can cause some temporary discomfort, but it usually goes away on its own. Pain medications may help. If it is especially bothersome, it may need to be surgically removed.
- Infections. Some men develop an infection after their vasectomy. The infection is usually treated with antibiotics.
- Hematoma. A hematoma occurs when blood collects in the scrotum after surgery. It often goes away on its own, but men should call their doctor if their scrotum gets bigger or becomes painful.
- Post-vasectomy pain syndrome. About 1% to 2% of men have chronic pain after vasectomy due to fluid buildup in the scrotum. Pain medications and warm baths may help. In more severe cases, surgery—or a vasectomy reversal procedure—may be needed.
Research shows that men who have vasectomies are not at higher risk for cancer or ED.
Does a vasectomy raise a man’s risk for cancer or erectile dysfunction (ED)?
No. Research shows that men who have vasectomies are not at higher risk for cancer or ED.
What is the vasectomy recovery period like?
Most men take it easy for a day or two after their vasectomy. There may be some pain and swelling, but these symptoms can be managed with pain medication and cold packs.
Men who work desk jobs usually go back to work the next day. Heavy lifting is restricted for about a week, so men with more physically demanding jobs may need to adjust their routine.
Men should avoid ejaculation—through partnered sex or masturbation—for about a week.
Is a vasectomy effective immediately?
No. It takes time for sperm cells to “clear” each vas deferens after a vasectomy. For this reason, couples need to continue using another form of birth control for a few more months or about 20 ejaculations.
After that period, men can see their urologist for a semen analysis. The doctor will check a semen sample for sperm cells. If some remain, couples should continue using birth control for a bit longer. If the semen is clear of sperm, other birth control methods should no longer be needed.
The best way to know whether sperm cells have cleared is to have a semen analysis with a urologist.
What happens to sperm cells after a vasectomy?
Instead of being ejaculated, sperm cells are absorbed by the body. This process is harmless.

What is sex like after a vasectomy?
Sex drive and orgasms feel the same as they did before the procedure. Semen volume should also be about the same, as sperm makes up a small percentage. Partners don’t feel a difference either.
Some men find sex to be more exciting after a vasectomy because they can be more spontaneous. The anxiety of unwanted pregnancy is reduced.
Does a vasectomy protect against sexually transmitted infections?
No. While vasectomies are extremely effective in preventing pregnancy, they do not protect against sexually transmitted infections (STIs) like HIV, HPV, and gonorrhea. Couples should still practice safe sex by using condoms and/or dental dams. Regular testing for STIs may also reduce the risk of transmission.
Can a vasectomy be reversed?
Yes. In general, vasectomy is considered a permanent decision, and men should think carefully before having one. But there are times when a man decides he would like to father children after all. That’s when a vasectomy reversal may be considered.
A vasectomy reversal procedure reconnects the ends of the vasa deferentia, giving sperm cells a clear path out of the body. (In some cases, the end of a vas may need to be connected to the epididymis, a coiled tube that links a testis with a vas deferens. The epididymis stores sperm cells.)
Vasectomy reversals are more involved than vasectomies, and they don’t always lead to pregnancy. Success can depend on how much time has passed between the vasectomy itself and the reversal. The longer the time frame, the less likely a pregnancy will happen.
It also takes time—sometimes a few months to a year—before sperm cells reappear in the semen.
Other factors, including a man’s overall health and the health and age of his partner, play a role in getting pregnant, too.
Besides vasectomy reversal, are there other ways to become a biological father after having a vasectomy?
Yes. It might be possible to retrieve sperm cells from the testes. These cells can then be used for in vitro fertilization (IVF).
Some men have their sperm frozen and stored by a sperm bank before their vasectomy, just in case they change their mind about fatherhood later.
Resources
American Urological Association
Sharlip, I.D., et al.
“Vasectomy (2015)”
(Published 2012; Amended 2015)
https://www.auanet.org/guidelines-and-quality/guidelines/vasectomy-guideline
“Vasectomy”
(Last updated: December 2020)
https://www.urologyhealth.org/urology-a-z/v/vasectomy
Mayo Clinic
“Vasectomy”
(August 21, 2021)
https://www.mayoclinic.org/tests-procedures/vasectomy/about/pac-20384580
UpToDate
Viera, Anthony J., MD, MPH
“Patient education: Vasectomy (Beyond the Basics)”
(Topic last updated: February 16, 2021)
https://www.uptodate.com/contents/vasectomy-beyond-the-basics



